Partner-Inflicted Brain Injury: Recognizing Invisible Injuries and Finding Hope for Healing

By: Elizabeth Clendenen, MSW Intern
This March, for brain injury awareness month, we want to draw attention to a less-visible group of people who are significantly impacted by brain injury. When we think about the people who are most affected by brain injuries, we typically think about football players and veterans. We don’t tend to think about survivors of intimate partner violence (IPV). However, survivors of IPV also experience high rates of brain injury and are impacted by brain injury in unique ways. Partner-inflicted brain injury is when person’s brain is hurt by strangulation and/or blows to the head that can cause a traumatic brain injury, concussion, or other type of brain injury while experiencing domestic violence. By learning more about the prevalence of partner-inflicted brain injury and its effects, advocates and healthcare providers can partner with survivors to make services more inclusive and trauma-informed for all survivors. Rachel Ramirez, the Founder and Director of the Center on Partner-Inflicted Brain Injury at the Ohio Domestic Violence Network (ODVN), spoke with me about this and the pioneering work that they are doing to educate providers and survivors and create resources to help prevent and treat brain injury.
Survivors of IPV experience high rates of brain injury in multiple forms. One study of individuals accessing shelter and community-based advocacy services conducted by ODVN and Dr. Julianna Nemeth, Assistant Professor at the College of Public Health at the Ohio State University, showed that 81% had been hit in the head and 83% had been strangled. Being hit in the head can lead to traumatic brain injury, where the brain is injured by rapid movement within the skull. Being strangled can lead to anoxic-hypoxic brain injury, where the brain is injured by partial or complete loss of oxygen to the brain. Both types of partner-inflicted brain injury can have serious physical and mental health impacts on survivors, including issues with memory and reasoning, seizures and tremors, noise and light sensitivity, nightmares and flashbacks, and difficulty controlling their emotions. These effects are exacerbated by repeated brain injuries, which is also common amongst survivors of IPV; the study referenced above found that 50% of survivors had been hit in the head so many times they had lost count. While some of the symptoms of trauma and partner-inflicted brain injury 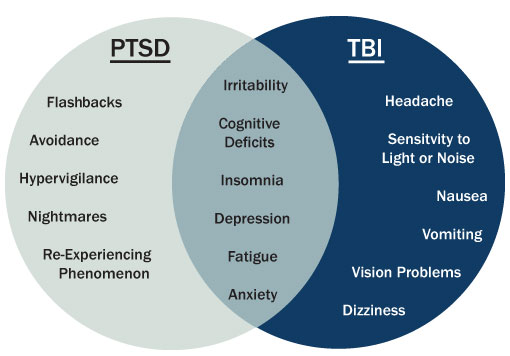 overlap, there are also many unique symptoms to each issue. It is important to recognize that the vast majority of survivors accessing program services are experiencing symptoms of trauma and brain injury. This is significant because treatments for post-traumatic stress disorder will not necessarily help with symptoms that are related solely to brain injury. Also, brain injury treatment will not help with trauma-related symptoms such as flashbacks, nightmares, and avoidance reactions.
overlap, there are also many unique symptoms to each issue. It is important to recognize that the vast majority of survivors accessing program services are experiencing symptoms of trauma and brain injury. This is significant because treatments for post-traumatic stress disorder will not necessarily help with symptoms that are related solely to brain injury. Also, brain injury treatment will not help with trauma-related symptoms such as flashbacks, nightmares, and avoidance reactions.
Given the emerging information we have about the prevalence and impact of partner-inflicted brain injury, advocates and healthcare providers can start taking steps towards better supporting survivors of IPV who have experienced partner-inflicted brain injury:
- Providers can start by learning more about the prevalence and impact of this issue and using resources to have conversations with their clients. Providers should begin raising awareness with survivors by making information and education available to survivors on these issues, as well as directly asking about and identifying head trauma caused by blows to the head and violence that restricted a person’s ability to breathe. Some tools developed by ODVN to provide education include the Head Injury Card and a booklet about Invisible Injuries. This is critical because most survivors who have a brain injury do not know they have a brain injury and often attribute symptoms they are experiencing to other physical or mental health conditions, the results of the trauma they have endured, or even personal character defects. Knowing that many survivors of IPV have experienced verbal and emotional abuse where they were insulted, degraded, and gaslit, helping survivors identify if they have experienced partner-inflicted brain injury and giving them resources to heal and thrive can be incredibly empowering. Advocates can use tools such as CHATS that help survivors identify symptoms that might be related to brain injury and provide structure for getting testing and treatment from their healthcare providers. Healthcare providers can use universal education approaches like CUES to talk to their patients about relationships and the health impacts of violence, including partner-inflicted brain injury.
 Providers should begin to look at service provision in a new light. Because a significant portion of survivors of IPV have experienced partner-inflicted brain injury and are dealing with the subsequent symptoms, we can create services and systems that account for this from the beginning – as opposed to making exceptions or accommodations for survivors who know that they have a brain injury and how it is impacting them. Traditional IPV service providers like shelters can create practices and policies that are more inclusive and trauma-informed for survivors who have experienced brain injury. This can include making shorter appointments, supporting survivors with organizing and remembering tasks, developing accessible written materials, and reframing how we understand survivors’ behavior. Just Breathe, a workbook focused on wellness and healing, gives survivors tools to prioritize self-care and emphasizes the importance of mental health alongside physical health. This workbook can also help programs learn what types of considerations and accommodations each individual survivor needs.
Providers should begin to look at service provision in a new light. Because a significant portion of survivors of IPV have experienced partner-inflicted brain injury and are dealing with the subsequent symptoms, we can create services and systems that account for this from the beginning – as opposed to making exceptions or accommodations for survivors who know that they have a brain injury and how it is impacting them. Traditional IPV service providers like shelters can create practices and policies that are more inclusive and trauma-informed for survivors who have experienced brain injury. This can include making shorter appointments, supporting survivors with organizing and remembering tasks, developing accessible written materials, and reframing how we understand survivors’ behavior. Just Breathe, a workbook focused on wellness and healing, gives survivors tools to prioritize self-care and emphasizes the importance of mental health alongside physical health. This workbook can also help programs learn what types of considerations and accommodations each individual survivor needs.- Finally, it is important to know that partner-inflicted brain injury is just one of the many possible health impacts of IPV. This should help motivate advocates and healthcare providers to develop stronger connections to better serve survivors. This can include advocates and healthcare providers building relationships, getting familiar with local services, co-hosting trainings, and providing in-house services (for example, a domestic violence advocate who visits a local health clinic once per week). These partnerships strengthen our ability to better service survivors of IPV experiencing health impacts such as brain injury. Check out www.ipvhealthpartners.org for step-by-step instructions and resources for building a health center and domestic violence agency partnership.
While this type of abuse can have challenging effects, it’s important to also emphasize that survivors can and do heal after experiencing partner-inflicted brain injury. The purpose of raising awareness about this issue is not to scare survivors or make them feel permanently damaged. The hope is that survivors will understand themselves better and receive services that are a better fit for their needs.
Relevant resources:





